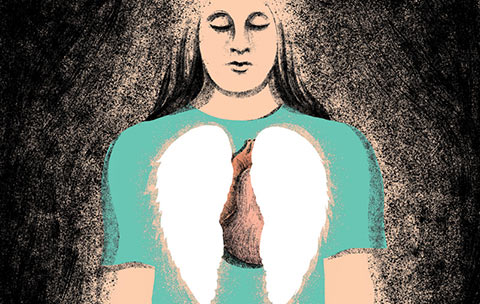
When Melissa Benoit woke up in hospital and learned she’d spent six days without lungs, she was stunned. “That blew my mind,” says the 33-year-old registered nurse from Burlington, Ontario. “I knew it was impossible for somebody to live without lungs. It made no sense.”
Benoit is believed to be the first in the world to undergo such a procedure. “We knew it was theoretically possible,” says Shaf Keshavjee, a U of T professor of thoracic surgery and the lead surgeon at Benoit’s operations. “But could a patient actually survive very long? That wasn’t entirely clear.”
The experimental procedure was a last-ditch attempt to save Benoit’s life. Born with cystic fibrosis, which affects the lungs and is the most common fatal genetic disease in young adults, Benoit had been battling H1N1 influenza. Then she contracted pseudomonas, a deadly bacterial infection. She quickly spiralled down into septic shock. Her blood pressure and oxygen levels plummeted. A lung transplant wasn’t an option at that point because having such severe sepsis made her ineligible. “We were very sure that if we didn’t do something radical, she would die that day,” says Niall Ferguson, a U of T professor of medicine and the head of critical care at the University Health Network (UHN).
While there was careful deliberation among the medical team before attempting the untried, her family was keen to proceed. Her husband, Chris, her parents and other relatives all agreed Benoit would grab any chance at life – especially in order to watch her two-year-old daughter, Olivia, grow up.
The initial operation took a 13-member team nine hours. “Lungs are normally soft and spongy, but hers were so filled with infection they were as hard as footballs,” says Keshavjee, who is also director of the Toronto Lung Transplant Program at Toronto General Hospital, part of UHN. Benoit was hooked up to two sophisticated cardiopulmonary life-support devices. One pumped blood out of her large veins, through an oxygenator and back into her aorta; the other served as the lung for the right side of her heart to pump through. “We were obsessive about maintaining blood pressure and oxygen levels to protect her brain,” Ferguson says. Within hours her condition stabilized. Although sedated and supported by the lung devices, Benoit was now eligible for a transplant. Six days later, donor lungs became available, and she underwent a successful five-hour surgery.
Benoit’s recovery has been, and still is, a long road. With her new lungs she can take glorious deep breaths without triggering the violent, rib-cracking coughing spells of the past. But, after more than three months’ immobility in critical care, she needed extensive physiotherapy to walk again. She takes many pills each day, including anti-rejection and anti-infection drugs. With cystic fibrosis–related diabetes and damaged kidneys, she’s on an insulin pump and dialysis and may undergo a kidney transplant, with her mom as donor.
But she’s full of gratitude for the dedicated professionals – and the deceased donor – who gave her her life back. She encourages everyone to register for organ donation at beadonor.ca. Tearing up, she says, “I wanted to present my story to the world because if there’s another family out there that has run out of hope, my experience might offer them a possibility.”
Could this procedure become routine? “It’s still very, very high-risk,” says Keshavjee, “but now we know it’s possible.”
Recent Posts
U of T’s 197th Birthday Quiz
Test your knowledge of all things U of T in honour of the university’s 197th anniversary on March 15!
Are Cold Plunges Good for You?
Research suggests they are, in three ways
Work Has Changed. So Have the Qualities of Good Leadership
Rapid shifts in everything from technology to employee expectations are pressuring leaders to constantly adapt