Craig Simmons, a U of T engineering professor, recalls having given a presentation not long ago about promising new heart research in children, when a mother came up to him crying. Her tears reflected the stress of being the parent of a child born with a congenital heart defect as well as gratitude that researchers like him were working on better solutions. “That really touched me,” says Simmons, who is scientific director of the translational biology and engineering program at the Ted Rogers Centre for Heart Research. It also motivated him as he continues his work on creating “living tissue” heart valves to replace defective ones in infants.
The Ted Rogers Centre – created through an unprecedented $130-million donation from the Rogers family – brings together more than 30 experts from Sick Kids, University Health Network and the University of Toronto to address heart failure across the lifespan. “We know Ted would have been proud of this bold initiative that will improve heart health for all,” says Loretta Rogers, wife of the late Ted Rogers.
We tend to think of heart disease as a problem in older adults, but children can have heart disease too. One in 100 babies in Canada is born with a congenital heart defect. In a healthy heart, the four valves open and close with every heartbeat, allowing blood to flow only one way. But a malfunctioning valve may leak, preventing a baby from getting enough oxygen-rich blood. This increases the risk for the child of infection, fatigue, fainting, delayed development, heart failure and sudden cardiac death.
The current treatment involves an initial surgery to repair or replace the defective valve in a tiny infant. Further complex operations are often required as the child outgrows the synthetic patch or valve, which are made of fabric, metals or plastics. But Simmons hopes “living tissue” heart valves that grow with the child will eliminate the need for those subsequent surgeries. “The kids would still need that single operation,” Simmons says, “but then they’d never need another.” Nor would they require maintenance medication such as blood thinners or anti-rejection drugs, as the new valve would be made from the baby’s own cells.
Simmons heads a research team focusing on growing replacement tissue for the pulmonary heart valve. The team harvests stem cells from a baby’s umbilical cord – typically discarded after birth – and attaches them to a polyurethane scaffold. Through chemical and mechanical stimulation – sort of like forcing the cells to do bodybuilding – the growing tissue becomes stronger and stiffer. Once implanted, the scaffolding would harmlessly biodegrade. Buoyed by early lab results, the team is now optimizing the processes for future animal testing.
“I’ve met people who as children had congenital heart problems – this past summer, one of them was a student who worked in my lab – and I’ve seen what an emotional burden this can be on children and families,” says Simmons. The costs to the health-care system are also significant.
Dr. Chris Calderone, surgeon-in-chief at Toronto’s Hospital for Sick Children and a professor in U of T’s department of surgery, is Simmons’ liaison in the clinical world. Together they’re focusing on a particular defect called Tetralogy of Fallot, where a baby’s first surgery takes place at four to six months. “This research could change the lifetime trajectory for these children, and also create a foundation for transferring this research to other valves in the heart,” says Calderone.

The Rogers Family
The Ted Rogers Centre for Heart Research was created through a $130-million donation from the Rogers family – the largest monetary gift ever to a Canadian health-care initiative. The centre has established an innovation fund to drive discovery and an education fund to attract a deep pool of talent for cardiac care and research in Canada.
Recent Posts
U of T’s Feminist Sports Club Is Here to Bend the Rules
The group invites non-athletes to try their hand at games like dodgeball and basketball in a fun – and distinctly supportive – atmosphere
From Mental Health Studies to Michelin Guide
U of T Scarborough alum Ambica Jain’s unexpected path to restaurant success
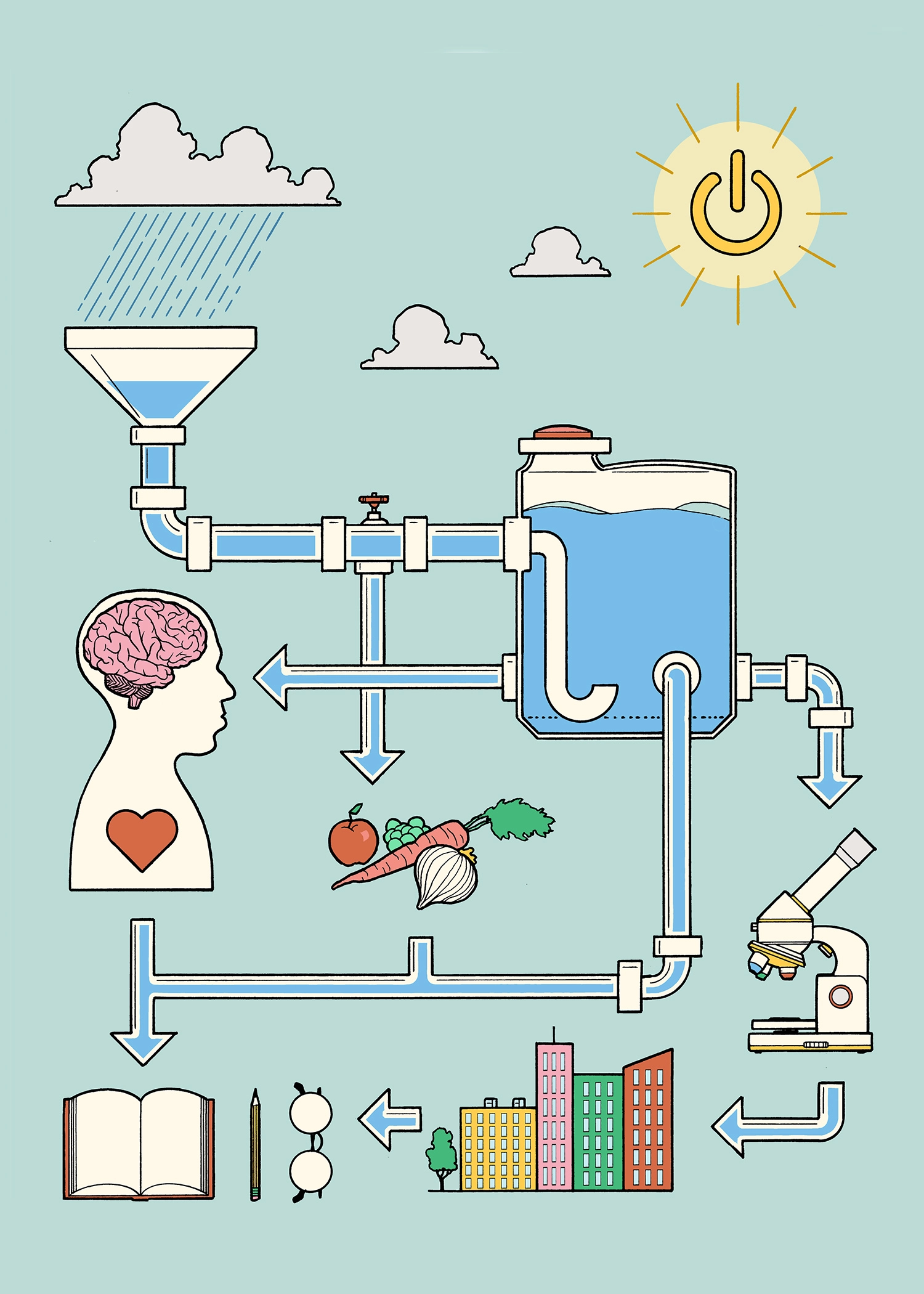
A Blueprint for Global Prosperity
Researchers across U of T are banding together to help the United Nations meet its 17 sustainable development goals





2 Responses to “ A Better Life for Children with Heart Defects ”
This is amazing. I am aware that infants and children can suffer from heart defects, and sometimes these defects go unnoticed. We are blessed with our daughters, today because of a surgery that was performed. I hope that many parents will be able to avoid all of the stress and anxiety that heart defects in their children cause.
May the new year bring you much success with this wonderful development, and may many children be saved from suffering and trauma because you have taken on the amazing responsibility of "mending hearts."
Terrific work led by a outstanding researcher. Great collaborative effort between engineering and medicine in the IBBME tradition.