Last summer, Leslie Cowan, a 41-year-old mother of two, left her home in Toronto, travelled to Buffalo, and checked into a medical centre to be treated with a cutting-edge cancer drug called Herceptin. The drug had shown encouraging results in the U.S., but hadn’t been approved in Ontario because of its high price tag: $35,000 to $45,000 per patient per year. To pay for her treatment, Cowan was prepared to remortgage her home, knowing she may no longer be able to help pay for university for her kids. But, as she said, “at least I’ll be alive.”
Herceptin is now available in Ontario, but its long journey to market underscores a profoundly difficult question for the people regulating the province’s strained health-care system. Do the overall benefits of such life-prolonging drugs exceed their considerable costs? For cancer patients, the answer is a resounding, ‘Yes, they do.’ But how much are we, as a society, prepared to pay for new drugs that purport to save – or prolong – a life? Is the sky the limit?
Dr. Murray Krahn, an associate professor in the department of Health Policy, Management and Evaluation at U of T, is an expert in cost-effectiveness analysis, a relatively young science that provides quantitative measures to help determine which drugs provide the most bang for the buck. “Cost-effectiveness analysis is kind of like a Consumer Reports for drugs,” says Dr. Krahn, the F. Norman Hughes Chair in Pharmacoeconomics. “It tells you whether a new drug is a good deal.”
In theory, says Dr. Krahn, cost-effectiveness calculations are straightforward. Analysts compare the cost of prescribing a new drug to the cost of using an older treatment – which could be a well-established pharmaceutical, or a combination of drugs and medical treatment. Experts in pharmacoeconomics then examine how the new therapy performs compared to previous treatments. They compare health benefits, such as long-term survival rates, tumour shrinkage, side effects and disease recurrence. The point is to assign a dollar value to the improved health promised by the new drug. This dollar value is what provincial drug plans should be willing to pay for the new therapy.
In practice, such calculations involve a complex array of clinical data and economic estimates. To illustrate the difficulty of such calculations, Dr. Krahn points out that a cost-benefit analysis of an everyday consumer product is tricky because value is a malleable and fundamentally subjective term. For example, is a Volvo worth more than a Hyundai? The price suggests that it is, but the extra value offered by a Volvo may not be worth the additional cost. It depends how you measure the benefits of owning a Volvo. “Shopping for a car is hard enough,” says Dr. Krahn. “Health is way more difficult. There are millions of diseases and millions of interventions.”
Consider a new osteoporosis drug that promises to reduce the incidence of hip fractures. Among patients who are prescribed the drug, one can presume that hospital expenses – emergency-room visits, surgery, nurses’ salaries, administrative overhead – will drop. You need to estimate the total reduction in hospital expenditures and weigh it against the cost of administering the drug.
Mike Tierney (BPharm 1978), the director of the Common Drug Review at the Canadian Coordinating Office for Health Technology Assessment, an independent agency that conducts such evaluations, says hospitalization costs can be estimated using data collected by the Canadian Institute for Health Information. The tricky part is that hospitalization rates vary significantly from province to province (and even from region to region) due to, for example, home-care policies and different treatment approaches. The point: the relative value of a new drug may vary depending on where it’s administered.
Even more difficult is gauging the effectiveness of a new treatment against previous therapies. Health Canada approves a drug based on how well it performs in experimental trials. The problem is that drugs behave differently in the real world, where a patient’s lifestyle – whether he misses pills, smokes, drinks, or dines predominantly on potato chips – can undermine a drug’s effectiveness. What’s more, trials offer limited data on how a new drug will fare in the long run. “This is one of the problems of going through with this kind of evaluation,” says Dr. Krahn. “People are called upon to do economic evaluations when the data isn’t as a mature as you’d like.”
Dr. Andreas Laupacis, president and CEO of the Institute for Clinical Evaluative Sciences and a drug evaluation expert in U of T’s Faculty of Medicine, cites the example of Iressa, a lung cancer therapy that was approved for use in 2003 on the basis of its promising performance in trials. “My understanding is that when it was evaluated in patients over the long term, the benefits were marginal,” he says.
The potential for miscalculation has some clinicians and epidemiologists complaining about the lack of standards in making evaluations, which are typically conducted by drug companies. Dr. Krahn says this skepticism is well deserved. “Cost-effectiveness evaluations are exponentially more complex from a design point of view than randomized controlled trials and more subject to the bias of the investigator.” In Australia, a 2000 review of 326 drug applications to the country’s Pharmaceutical Benefits Scheme found “significant problems” with two-thirds of the pharmacoeconomic evaluations conducted for the board, including biased or incomplete studies. In other words, evaluation experts may be basing decisions about whether or not to approve a drug on shaky economic analysis.
Equally contentious is what such studies actually reveal. When a new drug is subject to cost-effectiveness analysis, it results in a number that purports to tell policy-makers approximately how much extra cost a drug plan can expect to incur each year of a new treatment for one patient to achieve an improvement in quality of life. In a highly controversial 1992 paper that Dr. Laupacis wrote to provoke debate, he proposed that new drugs approved by Health Canada that have a net cost of less than $20,000 for each year of treatment per patient be deemed affordable and included on provincial drug plans, while those north of $100,000 be considered too pricey. “People asked, ‘Where did you come up with those numbers?’ The answer is, ‘We made them up.’”
Tierney insists that policy-makers don’t rely only on hard-and-fast thresholds to determine whether a new drug is too expensive relative to the benefits it provides. Still, many in the field regard $50,000 as the unofficial line separating overly pricey from affordable treatments. But, as Dr. Krahn observes, “No one knows what threshold we should be using. It’s a question of how we value some standard unit of health.”
With very expensive cancer drugs coming onto the market all the time, can Canada’s ailing health care infrastructure continue to bankroll these therapies without forcing financial sacrifices on other parts of society?
Most observers say the answer is political, but policy-makers still need to be able to tally up the actual costs and benefits. As Dr. Krahn puts it, cost-effectiveness evaluations are “a very powerful way of supporting decision-making.” Yet a pair of McMaster University health policy experts published a study in the Canadian Medical Association Journal in 2003 that cast doubt on whether cost-effectiveness analysis serves to contain overall drug expenditures. Arguing that the use of such evaluations is “a prescription for increased expenditures,” Amiram Gafni and Stephen Birch noted that the addition of a costly new drug to the provincial drug plan tends not to accompany cost reductions elsewhere in the system. As Dr. Laupacis points out, “Most drugs don’t replace older drugs; they expand the market.” In other words, as a greater number of drugs are approved, more drugs are being prescribed – and that means higher overall costs.
“What you fund is not a purely technical question,” says Dr. Peter Singer, the director of U of T’s Joint Centre for Bioethics and the Sun Life Financial Chair in Bioethics. Drug approvals must involve what he calls the “three Es” – evidence, economics and ethics. In his view, a cost-effectiveness assessment is necessary but insufficient. “The fundamental question is how much benefit a particular drug should have, and at what cost, before 13 million Ontarians are willing to pay for it,” he says. “There’s no straightforward answer.”
John Lorinc (BSc 1987) is a Toronto writer. His book The New City was just published.
Recent Posts
U of T’s Feminist Sports Club Is Here to Bend the Rules
The group invites non-athletes to try their hand at games like dodgeball and basketball in a fun – and distinctly supportive – atmosphere
From Mental Health Studies to Michelin Guide
U of T Scarborough alum Ambica Jain’s unexpected path to restaurant success
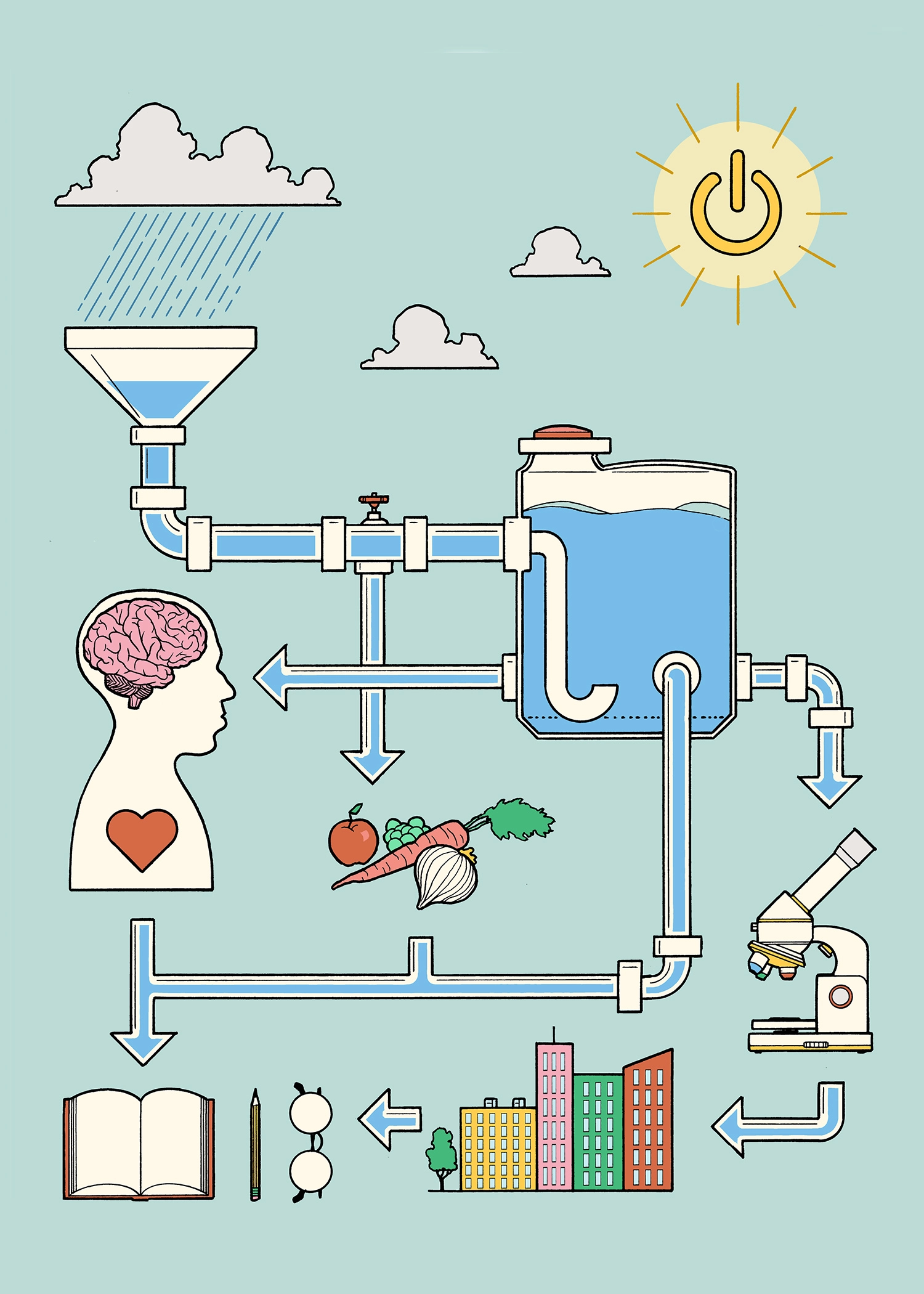
A Blueprint for Global Prosperity
Researchers across U of T are banding together to help the United Nations meet its 17 sustainable development goals