What can governments do to fight the escalating, and costly, health problems associated with the obesity epidemic sweeping North America and other developed countries?
The policies that have been tried so far – public education campaigns, additive bans, and taxes on high-fat and sugary foods – haven’t put a dent in the problem, say Massey College fellows Neil Seeman and Patrick Luciani. If anything, they argue in their new book, XXL: Obesity and the Limits of Shame (University of Toronto Press), some of these approaches waste valuable resources and even may have exacerbated the crisis.
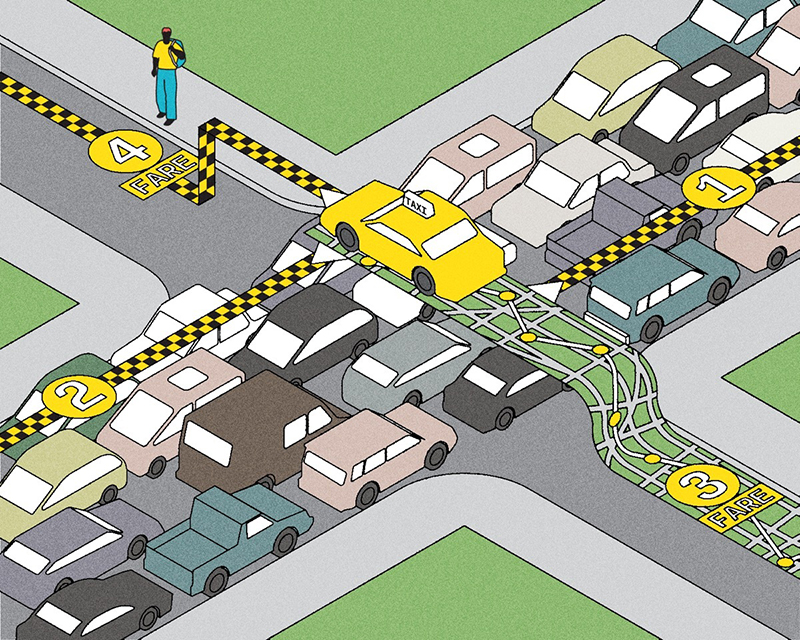
What’s driving the epidemic is a complex and interconnected list of factors that includes inactivity, the widespread availability of high-fat foods, city design that leaves us dependent on cars, and society’s unique genius for creating technologies that make life easier but also more sedate. It’s exceedingly difficult to isolate a single cause and effect, the authors say. Every obese person has their own story and their own struggle. “If we’re going to think seriously about obesity, we have to attack the problem at the individual level instead of using population-based approaches,” says Seeman. “These haven’t provided significant results.”
The authors’ alternative? “Healthy living vouchers,” which would reward people for purchasing health-related goods and services such as nutritious, low-fat food and gym memberships. Participants would be required to work with their primary health-care providers to develop a regimen geared at achieving long-term weight reduction. “It’s a preventative care model,” says Seeman, who has fought his own diet battles. “Everyone would take advantage of it.”
Currently, about two-thirds of Canada’s $230-billion health budget is directed to chronic disease treatment. Seeman and Luciani propose allocating between two and four per cent of Ottawa’s annual spending – $5 billion to $10 billion – to healthy living vouchers. Everyone over 16 would be entitled to participate, not just low-income people or those facing obesity problems. “The voucher is available to everyone because we want to encourage a sustained relationship between individuals and their doctors.”
The authors argue that their system would provide individuals with a direct financial incentive to improve their eating habits, their fitness level and their overall health. The vouchers would also engage market forces to allocate the resources needed to combat the obesity epidemic, rather than relying on government to determine the best approach.
Yet the system could also face nagging regulatory and political issues because it involves the transfer of hundreds or possibly thousands of dollars to every Canadian.
Seeman acknowledges that health spending could actually rise in the short term if the voucher system prompts patients to spend more time with their primary health-care providers (although the proposal would allow individuals to devise health plans with non-physicians). Another potential headache: determining which services and products should be included in the voucher program. Such a system may be vulnerable to special pleading. For those living in poor neighbourhoods with no fitness facilities, for example, the authors note that vouchers should be permitted to defray the cost of transit to gyms. But then why not gas costs, if they choose to drive?
Despite these objections, the authors argue that the obesity epidemic has become so pressing that governments have no choice but to be bold in searching for solutions. “The return on investment will not necessarily be seen in year one,” Seeman says.
Recent Posts
People Worry That AI Will Replace Workers. But It Could Make Some More Productive
These scholars say artificial intelligence could help reduce income inequality
A Sentinel for Global Health
AI is promising a better – and faster – way to monitor the world for emerging medical threats
The Age of Deception
AI is generating a disinformation arms race. The window to stop it may be closing




2 Responses to “ Your Loss is Your Gain ”
I am a Nurse Practitioner in the focus of Women's Health and Youth's Health as well as a Fitness Instructor Specialist. I love the concept and would love to be involved with making it happen!
I'd like to nominate healthy living vouchers as the dumbest health-related idea of the year.
The article starts by correctly listing the multiple causes of rampant obesity, lists some solutions, which Neil Seeman and Patrick Luciani deem ineffective, and then launches into their half-baked voucher proposal.
Certainly "...inactivity, widespread availability of high-fat foods, city design that leaves us dependent on cars..." are major contributors to obesity, and any solution must address these causes to be effective. The authors claim public policies have been ineffective. I would argue these policies will work, but have either not been initiated or sustained.
We are bombarded every day with advertising for stuff we don't need, but which will "make our lives easier." People forget our bodies are made for moving. I recall the Participaction ad campaigns from years ago. The average 30-year-old Canadian had the fitness level of a 60-year-old Swede. Why was this campaign cancelled? Why are recess and gym classes being cut out of junior schools? No wonder kids are having trouble paying attention in class. Now we drug them into submission.
Right from the start we are encouraging and supporting a sedate lifestyle. Marketing is a very effective tool. Look how fat we are! Positive and sustained campaigns for healthy living would be very beneficial. It is too bad that we have to be reminded to do the right thing, but even ads promoting good social behavior on public transit are effective. Supportive policies and education campaigns for healthy living must be done, and soon.
Some restrictive policy would also be beneficial. The authors talk about taxes on fat and sugary foods. Has this ever happened? Processed foods high in fat and sugar should be taxed higher than alcohol. The health effects on the population, and subsequent cost to our health care system, demand it.
Kids and adults are bombarded with hundreds of ads every day to eat fat and sugar. Parents have the opportunity to educate their kids about healthy food choices twice or maybe three times a day at mealtimes. We ban cigarette ads and put warnings on the packages because the cost of lung cancer treatment is excessive and burdensome to everyone. At the same time as healthy living is being promoted, ads for fat and sugar should be banned and restrictions placed on foods that have long term detrimental impact on the health of our society.
Along with public education and marketing for healthy living, broader policy changes are needed that challenge, among other things, our dependance on the car over other modes of transportation, allow urban sprawl, and reward unhealthy industries. Business, of course, will fight these initiatives, and unfortunately our politicians will capitulate. Building subdivisions creates jobs! Making cars creates jobs! Selling fat and sugar creates jobs!
There are, however, just as many other jobs that are less harmful to society if we dare to make the change, and as a society, it is time to look at the overall cost of our lifestyles. Healthy living vouchers are a band-aid at best for obesity if nothing else changes.
Martin Gagné
BASc 1984
Toronto