Physician-researcher Nav Persaud was worried. Several of his patients at the family practice unit in Toronto’s St. Michael’s Hospital weren’t getting better, despite having very manageable conditions such as high blood pressure, high cholesterol, HIV-AIDS or diabetes. The reason? They simply couldn’t afford their prescription medicines. “Some of my patients can’t afford insulin for their diabetes, even though they live in the city where insulin was discovered,” says Persaud, a professor in U of T’s department of family and community medicine.
Persaud and his fellow clinicians, many with similar patient experiences, considered their options. While the pharmaceutical samples they’d been giving out provided free meds for a week or so, they did little for chronic illnesses that required years of ongoing treatment. The doctors even considered pooling their own money to buy the necessary medicines, until they realized the problem required a bigger solution because it went far beyond their own patients.
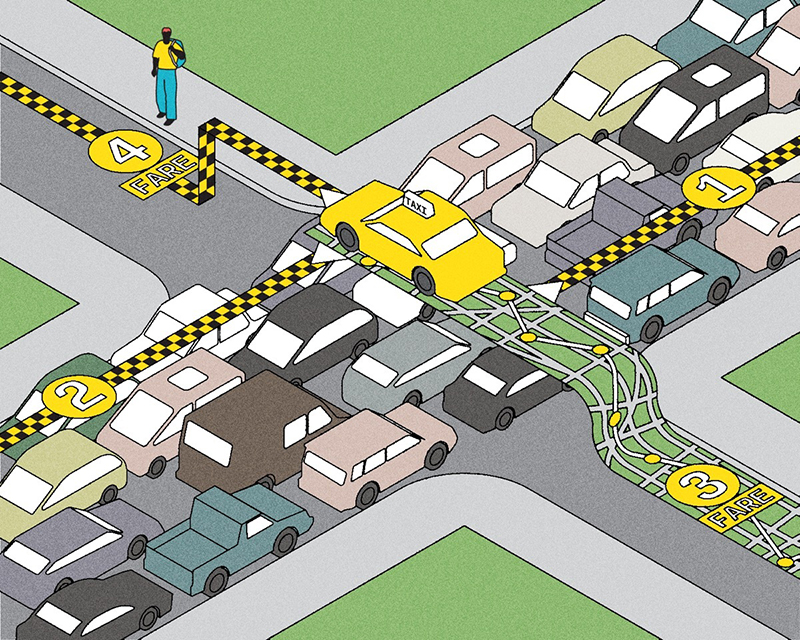
Almost two and a half million Canadians are in the same situation. Because of affordability issues, they take half doses, skip days or don’t fill their prescriptions at all. These may include people with no private insurance such as taxi drivers, restaurant servers, contract workers, farmers, artists, small-business owners and the unemployed, as well as those with workplace insurance who can’t afford the deductibles or who have topped out their maximum annual coverage. 1
Last year, Persaud’s team launched a two-year study to help inform public policy around universal pharmacare. The CLEAN-Meds study (Carefully seLected and Easily Accessible at No Charge MEDications) involves 786 patients in four family clinics in Toronto and at three sites in northern Ontario who had expressed difficulty affording medications. Half have been randomly assigned to receive their medicines free (mailed to their address for extra convenience), while half continue to have their usual access. The two groups will be compared for health outcomes as well as costs of the drugs versus costs of emergency room visits or hospital admissions. Preliminary results of the study are expected later this year. “We hope that by testing this program, we can inform public policy changes that would improve health and reduce health inequities across Canada,” says Persaud.
Many researchers are concerned primarily with the statistical results of their studies, but Persaud is also interested in following – and sharing – the lived experience of his patients. As part of his research, he is working with Open Lab at the University Health Network to create short videos of patients telling their own stories.
David, for example, owned his own company in the auto sector. On video, he speaks about how the 2008 financial crisis wiped out his business, taking him from “comfortably well off to desperate and living in my car.” A few years later, he underwent chemotherapy for lymphoma and recovered, but then had a heart attack. He skipped taking his meds because of stress over his financial situation, but now has his prescriptions filled through the study. “Stress is a huge killer,” he says. “It can exacerbate any illness. And to not have that stress every month has made me feel much, much better.”
The study’s quantitative results will eventually be posted to a website, but so will videos of David and four other patients – to give politicians and the general public a sense of the real-life impact of pharmacare, or the lack of it. “We’ll also ask patients to talk about what happens to them after the study ends, when they no longer get free meds,” says Persaud.
Excluding pharmacare from our universal health-care system is an accident of history, says Dr. Danielle Martin, a professor in U of T’s Faculty of Medicine. She says back when medicare was being built, most health care occurred in hospitals, where drug costs are covered. Now that medical science has turned many fatal diseases into chronic conditions, care has shifted into the home and community – with costs of medicines borne by an inefficient patchwork of private and public plans and individuals. It means doctors can examine, send for tests and refer to specialists, all with no direct cost to patients – but if treatment requires a prescription medicine, “all of a sudden they drop off the edge of the cliff in terms of what our publicly funded health-care system covers,” Martin says.
Canada is the only developed country that has public health care without universal pharmacare. Despite more than 13,000 approved pharmaceutical products, 137 medicines account for 77 per cent of all prescriptions. Persaud says a shortlist of essential medicines would focus competition on a small number of products that Canada could collectively purchase in larger quantities, saving Canadians $3 billion a year.
Recent Posts
People Worry That AI Will Replace Workers. But It Could Make Some More Productive
These scholars say artificial intelligence could help reduce income inequality
A Sentinel for Global Health
AI is promising a better – and faster – way to monitor the world for emerging medical threats
The Age of Deception
AI is generating a disinformation arms race. The window to stop it may be closing





2 Responses to “ The High Price of Pills ”
Ontario does have a universal pharmacare plan. It is called the Trillium Drug Program. Every Ontarian with a health card is eligible. You cannot be refused but you must apply. It is a means-based program, with a quarterly deductible based on your household income (never exceeding four per cent) making it extremely fair to recipients and taxpayers alike. It has been around for 20 years. Most provinces and territories have a pharmacare plan. Health care is a provincial responsibility. A national pharmacare plan would ignore the rights of provinces and make the existing infrastructure redundant. Is this a good use of tax dollars?
Dr. Nav Persaud responds:
It would be incorrect to say that Ontario has a "universal pharmacare plan." Most Ontarians are not enrolled in Trillium. Most would not benefit. Low-income people cannot afford the deductible and individuals must pay for their medicines until they pay the entire deductible. Other low-income individuals do not apply because they have not filed their taxes or for other reasons such as not being able to complete the forms. Most medium- and high-income Ontarians also would not benefit.
Trillium and similar programs in other provinces primarily benefit people with very high drug costs (e.g. someone earning $100,000 with drug costs of $25,000 a year). These catastrophic coverage plans are not universal pharmacare by any reasonable standard.
Millions of Canadians cannot afford medicines despite these programs. That would not be true if people just had to show their health card to get medicines (the same way they do for doctor visits, blood work, x-rays, surgery, ICU admissions).
Universal access to health-care services across Canada was implemented by the federal government via transfer funds to provinces. This is likely how universal pharmacare will be implemented across Canada.