As they enter their 60s, many people shift toward a different lifestyle, even if it isn’t complete retirement. But will this time of life be “such stuff as dreams are made on,” as Shakespeare wrote in The Tempest? Or will failing health prevent those in “the sixth age” from fully enjoying their lives?
Bombarded with media images of sixtysomethings reaping the rewards of wise investments, we tend to fixate on the monetary aspect of retirement. In reality, living the good life means not only having enough money but also being in good health and being able to spend time with others.
For more than 27 years Jury Kopach (BSc 1969, St. Michael’s) has helped companies prepare retirees-to-be for life after work. Kopach, a senior vice-president at T.E. Financial Consultants Ltd., says that once financial questions are settled, the focus shifts to health: “People become concerned about their longevity; they want to know if they will be around to enjoy their retirement.”
Statistically, a 65-year-old Canadian male can expect to live another 12 years, while a woman the same age can look forward to 16 more years of life. That’s plenty of time to do all those things you’ve been putting off – but also plenty of time for a debilitating illness to set in.
Unfortunately, some older people will face challenges that restrict their activity. Because women tend to live longer, they are more likely to experience the loss of a partner. Others may find themselves caring for extremely elderly parents, even as their own health is starting to deteriorate.
Men are particularly susceptible to loss at this age: the loss of prestige that came from their careers, the loss of physical abilities that can accompany age, the death of a spouse or close friend. These losses put them at high risk for depression, which may explain why suicide rates among older adults are nearly double those of adolescents.
Dr. Marnin Heisel, the Stephen Godfrey Fellow associated with the Arthur Sommer Rotenberg Chair in Suicide Studies in the department of psychiatry, recently developed an assessment measure – the first of its kind – that will help mental-health professionals identify seniors who have suicidal thoughts. The good news is that depression is treatable and should never be accepted as a normal aspect of aging.
Early identification is also vital in diagnosing osteoporosis, which typically begins much earlier in life but usually makes itself known in the sixth age and beyond. Hip and spinal fractures caused by fragile bones are especially common. Research shows that between 25 and 40 per cent of older people who break a hip may never walk unassisted again.
A major cause of disability among older people is osteoarthritis, a chronic condition resulting from years of wear and tear on bones and joints, among other factors. It’s estimated that 85 per cent of Canadians will experience some degree of joint pain and stiffness by age 70. Restorative surgery to replace worn-out hip and knee joints has been widely successful, and researchers have developed many strategies and devices that make it easier to live with osteoarthritis.
Half of all arthritis sufferers say they have pain that limits their activity. But they can improve their quality of life with the help of new medications and arthritis self-management techniques, says Dr. Elizabeth Badley, a professor in the department of public health sciences and director of the Arthritis Community Research Evaluation Unit (ACREU). Most important are proper exercise and healthy weight maintenance.
Recently Health Canada approved the use of COX-2 inhibitors, which may have less gastrointestinal toxicity than some other prescription medications for arthritis. These drugs may provide a useful option for osteoarthritis sufferers who aren’t helped by such traditional pain relievers as acetaminophen or ibuprofen.
One of the greatest fears of people over age 60 is that they will succumb to Alzheimer’s disease (see page 28). It’s true that the percentage of affected people doubles every 10 years after age 65, but occasional memory loss – which some ruefully call “having a senior moment” – is not an early sign of Alzheimer’s, says Dr. Fergus Craik, professor emeritus of psychology and senior scientist at the Rotman Research Institute at Baycrest Centre for Geriatric Care.
Craik explains that without a doubt, memory generally declines with age, but only certain types of memory are affected. Procedural memory – ability to read, drive a car, walk and swim – isn’t usually affected by normal aging. And knowledge of factual information also doesn’t deteriorate much, provided people remain mentally active. Instead, the greatest decline occurs in what’s called episodic memory: the recollection of personal events. As people age, they don’t encode their experiences as richly, says Craik, making it harder to retrieve memories, especially recent ones.
In the past 10 years, substantial advances in the care of the elderly have occurred. But as Dr. Michael Gordon, professor of medicine and head of geriatric and internal medicine at Baycrest Centre for Geriatric Care in Toronto, concludes, “We are getting better at postponing death, but we have not been as successful at eliminating diseases or reversing damage already done.” Gordon believes that the growing demographic of seniors is already setting much of the agenda for health care and research around the world, however, and the breakthroughs and developments along the way will be good news for us all.
Bred in the bone
Imagine one day being able to replace fragile bones with strong, new bone tissue cultured from a person’s own bone marrow cells. In fact, culturing human bone cells and new technologies for bone “scaffolding” are two recent breakthroughs from Dr. John Davies, a professor of biomaterials and biomedical engineering.
One of the major challenges in engineering bone and other tissue is coming up with the massive number of cells required. The use of bioreactor cultures (cell cultures that are prevented from coming into contact with surfaces) has overcome this obstacle. This technique keeps cells in suspension through continual stirring, promoting cell division while inhibiting further development. Vast numbers of precursor cells for human bone tissue can be introduced in this way. To transform these cells into active bone cells, they are extracted from the bioreactor, placed in a medium that encourages self-growth and attached onto a biodegradable scaffold.
This biodegradable scaffolding – a spongelike device – provides a structure to hold the cultured cells when they are placed in the body. As these cells grow and bone is regenerated, the scaffolding breaks down and disappears. While yet to be tried in humans, this bone-engineering process was tested on a laboratory rabbit missing a piece of its femur. After receiving the bioengineered bone tissue, it was up and hopping around within six weeks.
Recent Posts
U of T’s Feminist Sports Club Is Here to Bend the Rules
The group invites non-athletes to try their hand at games like dodgeball and basketball in a fun – and distinctly supportive – atmosphere
From Mental Health Studies to Michelin Guide
U of T Scarborough alum Ambica Jain’s unexpected path to restaurant success
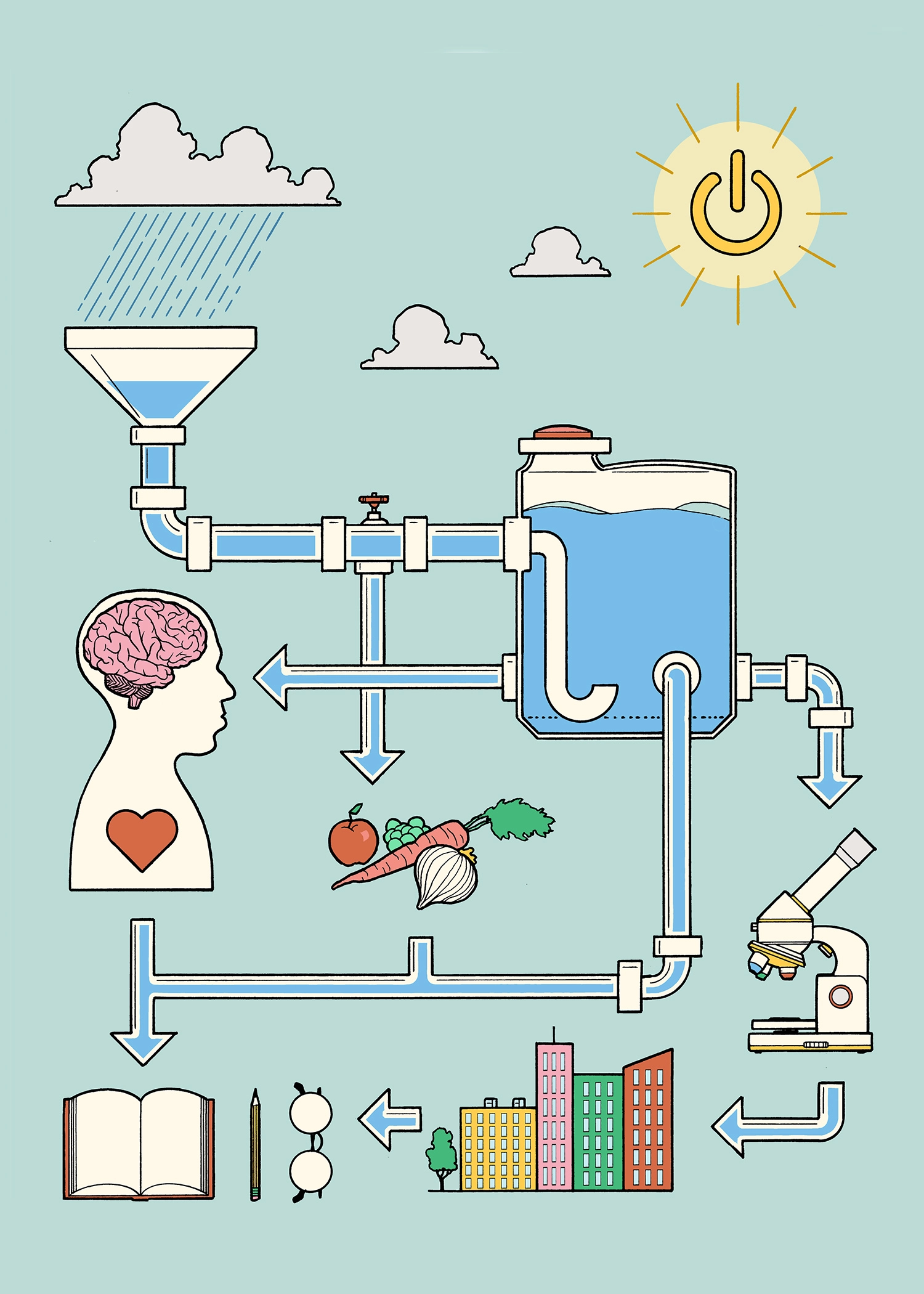
A Blueprint for Global Prosperity
Researchers across U of T are banding together to help the United Nations meet its 17 sustainable development goals