Almost half of adult Canadians say they have tried marijuana, a drug that has been illegal for almost a century. Nevertheless, many of us aren’t really sure what to think about the Trudeau government’s decision to legalize it. Public surveys show solid support for the use of marijuana for medical reasons. But for recreational use, views are mixed. While two-thirds of Canadians agree that the current laws need to change, there’s uncertainty about how that should happen, concern about the public health and societal implications, and much misinformation fuelling the debate.
Other jurisdictions around the world have reformed their cannabis laws: in 2013 Uruguay became the first country to fully legalize marijuana, the Netherlands has long allowed it in designated “coffee shops,” and four states – Colorado, Washington, Alaska and Oregon – have changed their laws to legalize pot sales and possession. Canada already has a system involving legal growers and medical marijuana users, and now we’re going to not merely expand that to recreational users but create an entirely new legal and regulatory apparatus. While that gives us a rare opportunity to design the best possible framework, it’s also a hugely complex undertaking.
“Legalization will help us minimize health risks and social harms,” says Jürgen Rehm, who is chair of addiction policy at U of T’s Dalla Lana School of Public Health and a professor of psychiatry. But with each province likely to be responsible for its own regulations, he warns that “the devil is in the details.” Rehm, who is also director of social and epidemiological research for the Centre for Addiction and Mental Health (CAMH), was involved with the creation of a policy framework featuring several “basic principles” – seen as minimum requirements – that aim to protect the public health in the event that cannabis is legalized. Here, we take a closer look at these principles.
1. Establish a government monopoly on cannabis sales. Set up control boards with a mandate for social responsibility to effectively control consumption and reduce harm. Limit availability by restricting the number of retail outlets and the hours of sale.
“Cannabis should be distributed through government-regulated retail outlets,” says Jenna Valleriani, a U of T doctoral student in sociology who studies legal and illegal cannabis markets in Canada. She suggests a retail model based on Ontario’s government-run LCBO liquor stores, where employees are trained to deal with a regulated product and to ban access to underage or impaired people – as opposed to over-the-counter access at a convenience store, as with cigarettes. This would help ensure that the product is quality-tested, consistent in THC content (tetrahydrocannabinol, one of the main chemicals that produces the cannabis “high”), and supplied only by government-licensed and regulated growers.
The premiers of Ontario and Manitoba support allowing provincially run liquor stores to expand their mandates and inventories to include marijuana, but Valleriani disagrees with selling both substances in one retail outlet. “I would be worried that people – particularly inexperienced users – would think it’s appropriate to mix them,” she says.
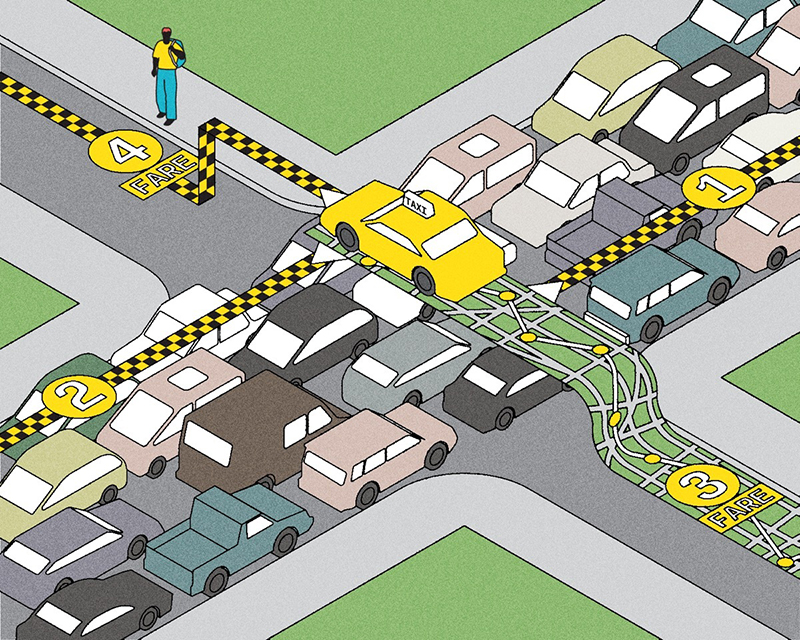
2. Establish prices that are high enough to curb demand but low enough to deter the continuation of a black market. Prices should also help steer buyers to lower-harm products.
We probably won’t be seeing weed on store shelves anytime soon, says Valleriani. It will take time to determine the optimal “Goldilocks” price point: not so low that recreational users will purchase it too frequently, and not so high that buyers will pursue cheaper product on the black market. Ontario’s experience with illegal cigarettes suggests that finding the right price for marijuana will be crucial to impeding illegal sales.
3. Set a minimum age for buying and using cannabis. Implement penalties for those who sell or supply cannabis to underage youth.
Despite the fact that marijuana is currently illegal, a UNICEF report in 2013 found that 28 per cent of Canadian children aged 11, 13 and 15 admitted to having used marijuana at least once in the previous year – the highest rate of all 29 developed countries in the study. “Cannabis is the easiest drug for young people to get their hands on, easier than alcohol or tobacco,” says Valleriani.
The new regulations will need to include several measures to help ensure that legalization doesn’t lead to greater access for youth. One of these is a minimum legal age to buy pot, which will probably be set somewhere between 18 and 21. Each province will likely determine its own age standards, but some research suggests older is better – even as high as 25. “An important goal for minimizing harm to youth is to delay use,” says Pat Erickson, a U of T professor in sociology and criminology who has studied the cultural and legal implications of cannabis policy for 40 years. “With a standard in place regarding minimum legal age, parents and teachers can speak to that standard.”
Why is it important to keep cannabis away from youth? Researchers have found a potential link between young people who use cannabis frequently and psychosis – an acute loss of contact with reality that can include delusions and hallucinations. “There is a very strong epidemiological association between cannabis use under the age of 16, heavy use and an increased risk of psychosis in vulnerable individuals,” says clinician-scientist Romina Mizrahi, director of the Focus on Youth psychosis prevention program at CAMH and a professor of psychiatry at U of T.
Vulnerable people include those who have a personal or family history of psychosis, but often there’s no way to tell who may develop psychosis. Mizrahi says that in an extremely sensitive individual, even occasional use may trigger an episode. “Since it’s difficult to know who will become psychotic and who will not, and since the brain is still developing during the teenage years, it makes sense for young people not to mess with the system where cannabis acts in the brain,” she says.
As for those who are caught selling marijuana to underage youth, Valleriani comments that penalties similar to what exist in Ontario for supplying minors with alcohol would seem appropriate – up to a $200,000 fine and one year in jail for individuals, and up to a $500,000 fine and suspension of the license to sell cannabis for companies.
She adds that penalties bring up other questions, too. For example: to what extent is the host of a party responsible for ensuring that underage guests don’t consume cannabis? Or, if adult guests consume it, that they don’t drive home? “There’s a lot to sort out,” she says.
4. Display product information clearly. In particular, products should be tested and labelled for THC and CBD (cannabidiol) content. Curtail higher-risk products, such as those with high THC formulations and products designed to appeal to youth.
Ruth Ross, chair of pharmacology and toxicology at U of T and senior scientist at CAMH’s Campbell Family Mental Health Research Institute, is a leading authority on how the body reacts to cannabis. She has conducted extensive research into the body’s endogenous cannabinoid system, which controls mood, memory, appetite and pain perception. As Ross explains, THC is the psychoactive ingredient in cannabis that, through its effect on the endogenous cannabinoid system, creates the “stoned” feeling. THC causes euphoria, increases appetite (“the munchies”), and mitigates pain and nausea; depending on the dose, it can also induce feelings of fear and paranoia. Ross says there is some evidence to indicate that CBD, another compound in cannabis, reduces some of the unpleasant effects of THC. CBD also has distinct pharmacological effects of its own.
A problem, says Ross, is that most of today’s recreational users cannot accurately determine the potency of the product before they use it. Nor can they be assured of its purity; it may contain contaminants such as pesticides and toxic fungi, says Ross. While the ratio of THC to CBD a generation ago hovered around 1 :1, with a relatively low percentage of each, today there’s a plethora of different ratios and percentages, she notes, some of them with much more powerful effects on the brain.
With a legal market, cannabis users may gain better understanding of what they’re buying. Still, there is some evidence to suggest that adolescents who are frequent users of potent cannabis may be more likely to develop mental health problems and may perform worse in school, so keeping all products away from youth is a good idea, says Ross. She adds that, due to the small number of good-quality, controlled research studies, it is difficult to make “robust statements” about the potential risks of cannabis use in adults.
5. Ban marketing, advertising and sponsorship. Products should be sold in plain packaging with warnings about health risks.
While provinces may be thrilled at the extra revenue from a marijuana sales tax, they must guard against the temptation to maximize profits, says Valleriani. We need to avoid the glamorization and commercialization of cannabis through advertising and promotion, she adds. “Nobody wants the Marlboro-ization of cannabis.” A portion of cannabis revenues should go toward public education as well as toward health care and support for harm-reduction services and rehabilitation, she says.
6. Develop a comprehensive framework to address and prevent cannabis-impaired driving. This should include prevention, education and enforcement.
Pot slows reaction time and alters distance perception, although some users deny it. Jürgen Rehm, who conducted a study involving U of T students who smoked marijuana and then underwent driving tests, says, “You would not believe how many people say they drive better after using cannabis. But we did objective measures and we showed very clearly their reaction time got worse. Nobody was better.”
In fact, impaired driving is the number 1 cause of cannabis-related mortality and is much more widespread than we might realize – likely causing hundreds of deaths and thousands of injuries in North America every year. Rehm says that in a recent study he did of people coming into the emergency room of Toronto’s downtown St. Michael’s Hospital with traffic-related injuries, more were impaired by cannabis than by alcohol.
Just as it took years to develop accurate breathalyzer tests for alcohol-impaired drivers, it will take time to create effective devices to test for cannabis impairment. This won’t be a blood test – “We don’t want police out there at the roadside with needles,” Rehm says – but most likely a saliva test. This can be done now, but research still needs to determine exactly what THC content indicates a person is unsafe to drive or to operate machinery. “We have to make sure the device is precise enough to withstand potential challenges in court,” he says.
7. Enhance access to treatment for cannabis use disorders and expand treatment options to include everything from brief interventions for at-risk users to more intensive interventions.
A little-known harm of marijuana is dependence. Although physical addiction has not been proven, about one in 10 users will develop what’s called a cannabis use disorder, manifested by a dependence that adversely affects their quality of life or functioning. (While 10 per cent is significant, the dependence figures for other drugs are much higher: 21 per cent for cocaine, 23 per cent for alcohol and 68 per cent for nicotine.) Each year, at least 75,000 Canadians seek treatment for cannabis use disorders – and that number may rise after marijuana is legalized.
Benedikt Fischer, a senior scientist at CAMH and a U of T professor of psychiatry, says treatment options for cannabis dependence are mostly limited to cognitive-behavioural therapy and other types of counselling. Unlike with alcohol, nicotine and opioids, there are no medications for cannabis dependence. “There are quite a few promising drugs, but we really have to ramp up research because we need more and better treatment options,” he says.
At the other end of the spectrum, Fischer says brief, evidence-based interventions are needed, particularly for young people who may begin experimenting with cannabis and may be at risk for problematic use. These interventions could be discussions with a knowledgeable professional at a doctor’s office or in a community setting or printed materials that provide information about the drug’s risks. Fischer notes that he and colleagues developed guidelines for lower-risk cannabis use, similar to those that exist for alcohol, which have been endorsed by the Canadian Public Health Association and other organizations. These include recommendations to use the drug less frequently than three times a week, avoid deep inhalation and not drive within four hours of using cannabis.
8. Invest in education and prevention programs. These should include general programs, such as to promote guidelines around lower-risk cannabis use, as well as targeted initiatives to raise awareness of the risks to specific groups, including adolescents and anyone with a personal or family history of mental illness.
Prohibition has meant that government funding for cannabis issues is directed much more to the criminal justice system than to health and education to create public education campaigns or harm reduction programs. This often leaves young people to experiment on their own without access to accurate information about cannabis – and youth, especially, are often uninformed about the risks of marijuana use.
The few campaigns that exist typically demonize cannabis use and focus on complete abstinence, says Fischer. What’s needed are educational materials that provide proportional information about cannabis use. “If you are using occasionally and you’re not driving, then this drug is not likely to cause you any serious harm,” he says. Fischer adds that it’s also important for youth to understand the relative risks of cannabis compared to, say, alcohol. “The impact of alcohol on brain development in young people is more severe than the impact of cannabis,” he says. “Few people talk about that. The impact of brain damage to young people in Canada from hockey-related injuries is extremely high. Few people talk about that. These relative risks need to be communicated broadly so young people are educated consistently and can make informed decisions.”
Fischer strongly supports the idea of using a portion of the money raised through taxes on marijuana sales to fund interventions and educational campaigns. “We need prevention campaigns for all age groups around cannabis and driving,” he says. “Most people still don’t understand the risks.”
Regulations will also need to cover the supply side of the equation. There are now 27 providers licensed by the government to sell to the 30,000-plus registered medical users. That market may jump dramatically; Health Canada has suggested it could reach half a million over the next decade, especially if covered by insurance plans. The recreational market is also expected to grow significantly. With hopes for an early foot-in-the-door into what will surely be a profitable industry, there are currently 1,400 applications from would-be producers, such as tech startups, waiting for Health Canada to sort through. The new regulations will need to limit how much influence the licensed companies will have. “It worries me to have only entrepreneurs at the policy table,” says Valleriani. “They are an important stakeholder, but not the only one.”
And what will happen to unlicensed growers, such as individuals who grow a few pot plants for their own use or to give or even sell to friends? That’s still a crime under the current laws, which is why some activists are calling for immediate decriminalization. Otherwise, some people may end up with criminal records while waiting for the promised legalization to happen. As it is, upwards of a million Canadians are estimated to be saddled with criminal records for marijuana offences, with tens of thousands of new cases every year (though only a fraction of these result in a conviction at trial or a fine). Enforcing cannabis laws costs Canadians an estimated $1.2 billion annually.
Not everyone is sold on the benefits of legalization, of course. Dr. Harold Kalant, a U of T professor emeritus of pharmacology and toxicology, has issued a 16-page critique of the CAMH policy framework, questioning, among other things, whether prohibition of marijuana has actually failed, whether it imposes serious harms on Canadians that would be removed by legalization, and whether legalization would eliminate the illicit market in the drug.
Nevertheless, by designing a comprehensive regulatory system for cannabis along with legalization, Canada looks set to become a trailblazer. But the change won’t happen all at once, and even after it happens, likely toward the end of the federal government’s term, there could be a long period of modifications and amendments. “I doubt we’ll get it right the first time, so we should be prepared to evaluate whatever policy the government puts in place and modify it,” says Erickson. “It’s going to be interesting times ahead.”
Recent Posts
People Worry That AI Will Replace Workers. But It Could Make Some More Productive
These scholars say artificial intelligence could help reduce income inequality
A Sentinel for Global Health
AI is promising a better – and faster – way to monitor the world for emerging medical threats
The Age of Deception
AI is generating a disinformation arms race. The window to stop it may be closing