It has been 44 years since Ana Osborne passed out one morning before school and woke up four hours later, bewildered. After dragging herself to the doctor and being ordered to get to a hospital immediately, the 18-year-old was diagnosed with Type 1 diabetes and told that her very survival would depend on frequent injections of life-saving insulin. An early routine involved poking her finger with a lancet, putting a drop of blood on a test strip to check her blood sugar level, and then using a syringe to inject insulin derived from a pig’s pancreas into the skin of her abdomen – multiple times a day. She has since tried so many different insulin types, tools and devices that her experience has almost mirrored the evolution of insulin therapy itself.
And today? Osborne wears a small disk-shaped sensor on her shoulder called a continuous glucose monitor. She uses a handheld device to read those numbers and she relays the information to a palm-sized computerized pump at her waist that delivers rapid-acting synthetic insulin under her skin via a tiny needle. “It’s much better than the older systems,” she says, acknowledging that even the best equipment is still a treatment, not a cure.
U of T researchers and their hospital partners recognize this as well, and are working on novel approaches to diabetes care that continue to improve lives for patients – building on something their predecessors started a century ago with the discovery of insulin. And for that, Osborne, who lives just north of Toronto, is deeply grateful. “If not for them,” she says, “I wouldn’t be here talking to you today.”
Back in 1921, Type 1 diabetes – once called juvenile diabetes – was a death sentence for the children and youth who developed it. There was no known cause, and the only treatment was a starvation diet that extended life by a few months. Into this reality came an ambitious young doctor named Frederick Banting, a farmer’s son from Alliston, Ontario. The youngest of five, he had struggled in school, flunking his first year of a general arts program at U of T’s Victoria College. Still, young Fred was serious and driven, and since the country was in dire need of doctors, he was accepted into medical school. After graduating, he served as a medical officer in England and France during the First World War. When he returned to Canada, he took a year of surgical training at Toronto’s Hospital for Sick Children. Then, unable to find a full-time staff job, he opened a small medical practice in London, Ontario. The patients were slow to arrive. Banting’s practice faltered, and he fell into debt. He picked up part-time work teaching at the University of Western Ontario (now Western University) but still could not pay his bills.
It was around this time, while preparing a lecture for medical students about the pancreas, that Banting decided to pursue a middle-of-the-night idea he’d had about curing diabetes. With no laboratory available at Western, he persuaded a reluctant John Macleod, a professor of physiology at U of T and an expert in carbohydrate metabolism, to give him lab space over the summer of 1921, along with a research assistant. The assistant turned out to be Charles Best, 22, newly graduated from U of T in biochemistry and physiology. Banting closed his medical practice and moved to Toronto. As he and Best conducted experiments under Macleod’s direction, they realized Banting’s hypothesis about curing diabetes didn’t work. They did discover, however, that injecting diabetic dogs with an extract made from the animals’ own surgically removed pancreases dramatically lowered the animals’ blood sugar levels. Aha! They knew they were on to something. They just didn’t know how to purify this extract to make it safe for human clinical trials.
Macleod invited University of Alberta biochemist James Collip, who had returned to his alma mater, U of T, for a sabbatical, to work on the purification process. Within weeks, using the pancreases of cattle from slaughterhouses, Collip figured out a way to purify the extract – now called insulin – by using a high concentration of alcohol.

Days later, the first recipient of an injection was Leonard Thompson, a 14-year-old patient at Toronto General Hospital weighing only 65 pounds and close to death. The boy responded quickly and recovered well. When the dying teenage daughter of then U.S. Secretary of State Charles Hughes rebounded to rosy-cheeked health after insulin treatment in Toronto, the international press went wild. Banting became a celebrity. He and Macleod received the Nobel Prize just one year later. Banting, upset that Best had been passed over, split the prize money with his young assistant. Macleod did the same with Collip.
In January 1923, the team of Banting, Best and Collip assigned insulin patent rights to U of T as a public trust for the symbolic amount of one dollar each. As Banting said, “Insulin belongs to the world, not to me.” The university’s insulin committee then licensed pharmaceutical companies to produce and distribute insulin, primarily in North America, at a royalty rate of five per cent. By the summer of that year, U of T’s Connaught Laboratories was producing 250,000 units of insulin a week for use in Canada and internationally.
Now, after 100 years, the world needs insulin more than ever. Almost half a billion people worldwide live with Type 1 or Type 2 diabetes – a number expected to soar over the next decade due primarily to rising rates of obesity. 1 And while it’s no longer imminently fatal, the disease still kills approximately 1.6 million people every year. 2 Researchers continue to focus on ways to improve – and save – patients’ lives. “There have been, and continue to be, tremendous advances that have positively impacted the lives of people with diabetes,” says Gary Lewis, director of U of T’s Banting and Best Diabetes Centre and a senior scientist at the Toronto General Hospital Research Institute. While there is still no cure, he says U of T researchers and their hospital partners are getting closer all the time. “One kind of cure [for Type 1 diabetes] could come in the form of stem cell therapy, another in immune therapy.”
In Type 1 diabetes, an autoimmune disease usually acquired in childhood or adolescence, the immune system mistakenly kills the body’s beta cells, which produce insulin – the hormone that regulates our blood sugar levels. In Type 2 diabetes, the body either doesn’t produce enough insulin or can’t use it properly.
You might think that a transplant, of either an entire pancreas or just the islets (clusters of cells within the pancreas that include beta cells), would be an answer to curing Type 1 diabetes. But there are problems: there is always a shortage of donors; islet transplant requires two or three donors because many cells are damaged in the process; and recipients must take immune-suppressing drugs for life. These drugs carry risks of cancers and infections.
But what if we could find an unlimited source of islets that would also eliminate the need to take immune-suppressing drugs? One U of T team in the field of regenerative medicine is working on exactly that. Under Cristina Nostro, principal investigator at the McEwan Stem Cell Institute at the University Health Network, researchers start with pluripotent stem cells (informally known as cells that can “be whatever they want when they grow up”). Scientists can take these cells, and with the addition of various proteins, instruct them to behave like islet cells. The problem: if your body attacked your own islet cells (which include beta cells) before, it will attack these cells, too. A research group at the University of Washington Seattle is collaborating with Nostro on making these cells invisible to the immune system, she says. “Then we could transplant without the need of immune suppressants.”
The Washington team is taking three approaches to achieve “invisibility.” Meanwhile, Nostro’s team is working to demonstrate that these “instructed” islet cells actually function like islet cells and will not be rejected by the immune system. With patents filed and strong connections forged with Toronto General Hospital (and its ready supply of patients and surgical expertise), Nostro, also a professor in the department of physiology, is hoping to one day launch a clinical trial in Toronto. “I’m super excited,” she says. “The progress we’ve made is extraordinary.”
Another U of T team is working on tricking the immune system by manipulating T-cells, a type of white blood cell that, in Type 1 diabetes, mistakenly attacks healthy islet cells. Under Juan Carlos Zúñiga-Pflücker, a professor in U of T’s department of immunology and a senior scientist at Sunnybrook Health Sciences Centre, the team is using a specific protein to convert the misdirected T-cells into regulatory T-cells, which suppress the immune system and can prevent autoimmune disease. Zúñiga-Pflücker has co-founded a company, Notch Therapeutics, to bring this technology to market. “If you measure antibodies, which can identify children and young adults who haven’t yet developed diabetes but who are at high risk, modulating the immune system can prevent the total destruction of those cells and prolong their function,” Lewis says.
Other U of T research teams are focusing on Type 2 diabetes, which is much more common than Type 1, and much more closely linked to lifestyle. “There’s no question that if we solve the problem of obesity, we can solve most of the problem of Type 2 diabetes,” says Lewis. But obesity is a complex global epidemic that involves far more than simply choosing to eat too much or exercise too little. It’s partly genetic: Asian, Black, Hispanic/Latino and Indigenous populations have a higher risk of obesity and diabetes. It’s partly biological, with our natural human attraction to fatty and sweet tastes and our evolutionary ability to store fat. It’s partly our modern society, which necessitates sedentary, screen-based work or school. And it’s partly the social determinants of health: socioeconomic inequalities leave disadvantaged people without access to nutritious food, recreation opportunities, medical specialists or healthy outlets to manage stress. Lewis says, “In Type 2 diabetes, the social determinants of health totally swamp the genetic and biological determinants.” And they are affecting younger people. An alarming 2020 Manitoba government study found that the rate of Type 2 diabetes among children in Indigenous communities in that province is 25 times higher than that of other children. (See U of T Mississauga Opens a New Centre for Diabetes Research)
The link between stress and diet has been a particular research interest of Jacqueline Beaudry, an assistant professor in the department of nutritional sciences. She found that giving rats elevated stress hormones raised their blood sugar a little, but combining that with a high-fat diet gave them diabetes within one to two weeks. “It was very shocking,” Beaudry says. (Her PhD on the subject won the Governor General’s Academic Medal in 2014.) It is known that people who have high stress hormones tend to accumulate fat around their mid-section. But how much control do we have over our stress hormones? “We’re struggling with that all the time – especially going through a pandemic.” 3
Beaudry is now studying how various hormones affect our fat tissue, which is a major regulator of whole-body metabolism. Stress hormones target different types of fat differently; they seem to particularly target fat around our abdomen, but we don’t fully understand why. Not all fat is bad, she says. Unlike harmful white fat, brown fat is packed with energy-producing mitochondria. The presence of brown fat is also associated with lower amounts of central body fat and a lower likelihood of diabetes. “Learning more about how stress hormones target different types of fat may give us insight into how to prevent or manage the onset of chronic diseases such as obesity and Type 2 diabetes,” she says.
Bariatric surgery used to be the only effective treatment for permanent weight loss, but Lewis says it is invasive, risky and associated with long-term complications. It likely will be phased out as medical therapies for obesity improve. There are now two medications that help people lose a significant amount of weight safely. One mimics GLP-1, a gut hormone that slows digestion, lowers blood sugar, suppresses appetite, reduces weight and protects the heart. The other is a SGLT2 inhibitor, which also lowers blood sugar and protects the heart, although weight loss is often more modest.
There are also diabetes initiatives across the country. Diabetes Action Canada, under Lewis’s direction, is a national consortium of more than 100 researchers. The group teams up with people living with diabetes and their caregivers to learn how to prevent diabetes and its complications and to improve patient care in a variety of ways.
Even after 100 years, there is still no cure for diabetes. But Lewis is hopeful one is on the way. Meanwhile, treatments continue to improve dramatically. “If you develop diabetes in 2021, your life and your life expectancy are completely different than they would have been in 1921,” he says. “It’s a very exciting, very hopeful time.”
This version of this story corrects an earlier one stating that U of T had licensed insulin royalty-free to pharmaceutical companies around the globe. In fact, U of T earned royalties from insulin. The university’s insulin committee gave full patent rights for the United Kingdom to the Medical Research Council there, and facilitated production agreements in various other countries.
For a much more detailed account of insulin’s discovery, visit Defining Moments Canada.
Igniting a Century of Discovery
U of T and its partner hospitals have built a culture of innovation that has brought about major advances in health care. Here are some of the most important discoveries made by doctors and scientists affiliated with U of T in the past 100 years.
1921
Frederick Banting and Charles Best discover insulin

1925
 The discovery of insulin spurs growth in Connaught Laboratories and public health education, leading to the creation of U of T’s School of Hygiene
The discovery of insulin spurs growth in Connaught Laboratories and public health education, leading to the creation of U of T’s School of Hygiene
1943
Leone Farrell’s research makes possible the large-scale production of the polio vaccine

1951

Wilfred Bigelow develops the first electronic heart pacemaker
1961
James Till and Ernest McCulloch discover the blood-forming stem cell, which becomes the basis for regenerative medicine
1975
Vera Peters revolutionizes the way we approach cancer treatment by showing that treating early-stage breast cancer with lumpectomy and radiation is just as effective as radical mastectomy

1981
David Jenkins develops the Glycemic Index, which enables people to manage their blood sugar level through diet
1984
Tak Mak helps to identify the T-cell receptor gene, a major advance in understanding the body’s immune system
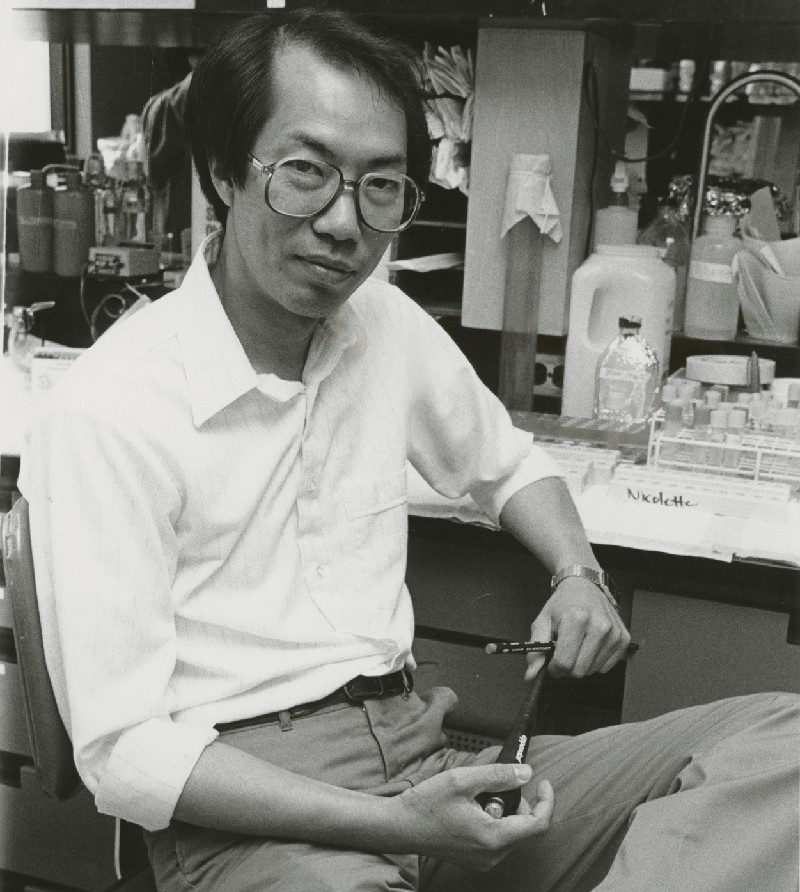
1986
Dan Drucker identifies the role of gut hormone GLP-1 in control of insulin secretion, eventually leading to new drugs to treat diabetes
1988
Alan Hudson and Susan Mackinnon perform the first nerve transplant
1994
John Dick identifies cancer stem cells
2010
 Derek van der Kooy uses stem cells to restore sight in blind mice
Derek van der Kooy uses stem cells to restore sight in blind mice
2013
Milica Radisic becomes the first to use electrical pulses to turn stem cells into mature cardiac cells, signalling a significant advance in tissue engineering



13 Responses to “ The Miracle of Insulin ”
I'm pleased to see you referenced Frederick Banting's First World War experience.
A most interesting article!
However, it would have been nice to see the author mentioning the book The Discovery of Insulin by Michael Bliss who was a U of T grad and long time history professor!
I would hope that the author consulted that award winning book!
Thanks for sharing this amazing discovery. I heard about Banting and Best from one of my professors at Ramsay. Wishing U of T success.
I am 87 years old. I graduated from U of T as an actuary in 1955. My mother's father, Abraham Sherman, was one of the first people to be saved by the Banting and Best discovery. He decided to retire at age 44, and spent a lot of time with me, taking me to Toronto, Michigan, Lake Simcoe. This was wonderful because my mother and father worked hard and didn't have much time for me. He even taught me to drive a car and how to operate a boat -- none of which would have been possible without insulin.
My son attended U of T for two years. During his time there, we were able to visit both the U of T exhibit and the Banting House Museum in London, Ontario. Banting House Museum goes into more details about Banting’s life. I highly recommend both!
Thank you for your interesting article. Gladys Boyd, my mother's first cousin, graduated from the University of Toronto in 1918 with a Bachelor of Medicine. She was appointed the head of Endocrine Services at the Hospital for Sick Children in 1921 and held this position until 1950.
Fredrick Banting stated in his Nobel Prize Lecture, “With the improvement in the quality of insulin, the increased knowledge of its physiological action and the increased quantities at our disposal ... a clinic was established ... at the Toronto Hospital for Sick Children in association with Dr. Gladys Boyd” in 1922.
In that year alone, 18 diabetic children benefited greatly from insulin treatment in the clinic she oversaw.
On p. 103 of the Frederick Banting biography by Michael Bliss, it states, “One notable case at Sick Children’s was an eleven-year-old Canadian girl, Elsie Needham, diabetic for six months, who gorged herself on grapes and olives one day in October [1922] and was brought into the hospital in coma. Comatose diabetics died. Banting and Dr. Gladys Boyd gave the girl insulin. It drove her blood sugar so low that Banting got cold feet and gave her sugar. After days of insulin, enemas, fever, delirium and roller-coaster changes in her condition, Elsie Needham regained consciousness.”
The Discovery of Insulin, also by Michael Bliss, notes, “By January [Elsie] was back in school, to all appearances a healthy, normal child, with years of life ahead of her.” Dr. Banting recorded that “She was the first child to recover from coma by the use of insulin."
Three of six diabetic children who were in comas recovered with the use of insulin in 1922.
The Manual for Diabetics (1925) was authored by Gladys Boyd and Marion Stalsmith (with an introduction by Banting). It was provided to all patients/parents attending the Diabetic Clinic at Sick Kids. It also became the standard text for the public.
As one of the first physicians worldwide to treat diabetic children with insulin in the clinical setting, Dr. Boyd became an early international authority on the management of this disease in children.
Dr. Boyd’s legacy is reflected in the fact that, according to Defining Moments Canada, the SickKids Endocrine Department now assesses close to 100 children and adolescents with new-onset diabetes annually, as well as over 800 who receive comprehensive tertiary care.
I have had Type 1 diabetes for 63 years and have followed all the treatment changes. Your article was very interesting and I especially appreciated the summary at the end. Improvements in monitoring have helped to make life better for people with diabetes but they are not a cure. This anniversary helps reminds us that there is still a long way to go.
Thank you for this refreshing outline of the historical research and development to alleviate diabetes, as well as information about other medical breakthroughs.
During the pandemic, this story helps underscore the importance and promise of scientific research.
Another milestone: the January 1939 patent for protamine-zinc insulin, which was developed at Connaught Laboratories in the 1930s by Dr. D. A. Scott and Dr. A. M. Fisher.
"The effect of protamine-zinc insulin is characterized by a relatively retarded lowering of the blood-sugar level and maintenance of a low level for an extended period. In a very large number of instances this prolonged effect is of great benefit and reduces or eliminates the need for multiple daily injections." Jamieson et al, Cdn Med Assoc J. 65, 1951, p.20-23.
Drs. Scott and Fisher also developed crystalline insulin, which replaced amorphous insulin by 1940. Patent royalties, administered by the university's Insulin Committee, were a major source of income to support further research at Connaught. Dr. Albert Fisher was my father.
A fine article. Not mentioned however was the significant partnership U of T has with Defining Moments Canada who are leading the national commemoration for "Insulin100" under contract with the Ministry of Canadian Heritage and multiple other partners across Canada. We were proud to share the stories of Dr(s) Banting, Best, MacLeod & Collip, but also very proud to feature the stories of Dr. Gladys Boyd and many lesser-known but equally significant leaders in insulin research over the last century. All freely available at: www.definingmomentscanada.ca.
Allan Levine (MA 1979, PhD 1985) writes:
There is a glaring omission in this otherwise excellent article: any mention of the late Prof. Michael Bliss’s ground-breaking 1982 book, The Discovery of Insulin.
A long-time member of the university’s history department, Bliss’s prodigious research confirmed that Frederick Banting, Charles Best, James Collip and J.J.R. Macleod all played key roles in the miracle. The book also became the basis for the acclaimed 1988 Canadian film, Glory Enough for All.
I suspect the writer, Marcia Kaye, must have used The Discovery of Insulin as a reference. If so, the article might have noted that.
There is an error in this piece. It says “ The team sold the patent to U of T for a dollar, and the university then licensed it royalty-free to pharmaceutical companies around the globe.” The university did in fact receive ample royalties as reported by the Washington Post in 2016. Here is an excerpt: “"It has come to be universally recognized over all the civilized world that the university has performed a great service for humanity," the Scottish biochemist John J. Macleod, who shared the Nobel Prize for insulin, said in 1924. In a statement to Toronto's Insulin Committee, he praised the scheme the university had developed prevented the 'commercial exploitation' of the essential drug. But with a 5 percent royalty on insulin, the university had already amassed $10,000.”
@Erin
Thank you for bringing this to our attention. The error has now been corrected.